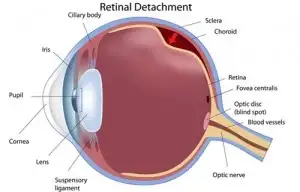
Retina is like the film in a camera. Retina is the third and inner coat of the eye which is a light-sensitive layer of tissue. When the focused light hits the retina, a picture is created and sent to the brain through the optic nerve (the nerve of the eye), thus giving us vision. Sometimes part of the retina either tears, pulls away or detaches from the back of the eye; when this occurs that part of the retina cannot gather light ans results in vision loss.
Retinal Tears Explain By Dr. Niteen Dedhia @ Ojas Eye Hosital
During normal aging, yellowish deposits, called drusen, form under the retina, which is the light-sensitive layer of tissue at the back of the eye that provides clear, sharp images.
As drusen increase in size and number, they can interfere with proper functioning of the retina, damaging or killing the light-sensitive cells of the macula.
Because the macula’s light-sensitive cells provide the ability to have sharp, detailed vision, the results can be blurring of central vision and a devastating impact on the ability to enjoy activities of daily life, such as reading, driving, or even recognizing the face of a friend or family member.
This form of age-related macular degeneration is called dry AMD. Dry AMD can be a precursor to wet AMD.
Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These blood vessels often leak blood and fluid, damaging or killing light-sensitive cells — loss of vision occurs quickly.
Although approximately 80 percent of patients with age-related macular degeneration have dry AMD, wet AMD is responsible for 80 to 90 percent of severe loss of vision with this disease.
AMD may be a difficult condition, but it is not as devastating as people fear when they are diagnosed and only rarely leads to complete blindness. Millions of people actually live healthy, independent lives, despite having age-related macular degeneration.
It is important to learn about the disease and work with a retina specialist, who will put a treatment plan in place. These physicians have the ability, training, and experience to treat all medical and surgical aspects of AMD and other diseases of the retina.
A retina specialist can also suggest access to rehabilitation options like low vision aids which includes a variety of tools and resources that can make everyday living with AMD a little bit easier.
The earliest signs of AMD in the retina can be detected by a retina specialist before you have any vision loss, but those who have had the disease for some time may notice changes in vision which are symptomatic of dry and wet AMD.

Early stage wet AMD

End stage wet AMD with scarring
It is important to pay close attention to any decline in central vision — both near and distant. If you notice any of these signs or symptoms, schedule an examination with a retina specialist.
Many people ask if age-related macular degeneration can be prevented. Like most things in life, there is no easy answer.
The primary risk factor for AMD is age — the older you are, the greater your risk. Also, people with a family history of AMD are at higher risk, as are women and people of European descent.
Some lifestyle factors are also known to increase your risk for AMD:
The best way to detect AMD is an examination by a retina specialist. The following are some typical methods he/she will use to check for AMD.
In this examination, a physician uses eye drops to dilate, or widen, the pupil to examine the retina. Regular dilated eye exams are important, especially for those who are at a higher risk for developing AMD.
If you are over the age of 50, it is a good idea to schedule a periodic eye examination to look for the earliest signs of AMD before any vision loss has occurred.
The physician may suggest an optical coherence tomography (OCT) exam. This test provides cross-sectional images of the retina that show its thickness, helping determine whether fluid has leaked into retinal tissue and other changes that happen with AMD.
Another way to detect AMD is by using an Amsler grid test. In this test, the patient covers one eye at a time and stares at the black dot at the center of the grid. If the straight lines appear broken, crooked, wavy, bent, or distorted, the patient may have AMD.
It is important to note that this test is hardly sufficient to rule out the possibility of AMD, as many people with the disease may see no abnormalities on an Amsler grid.
Because AMD affects visual acuity, an eye chart can also be an indicator of the development of AMD.
There is no known cure for AMD, but early detection and proper treatment can protect vision from further deterioration.
There is a variety of medical treatments that can help stop further vision loss caused by wet AMD:
Tears or detachment results from aging, an eye-injury, or another eye problem.
A retinal detachment occurs when fluid leaks through the tear and separates the retina from the back of the eye.
Treatment of Retinal Tear is mainly surgical this involves :
This procedure can be used to treat retinal detachment if the tear is small and easy to close. A small gas bubble is injected into the eye (specifically into the clear, gel-like substance between the lens and the retina), where it then rises and presses against the retina, closing the tear. A laser or cryopexy can then be used to seal the tear.
Each of these treatments seals the retina to the back of the eye, and prevents progressive deterioration of the tear.
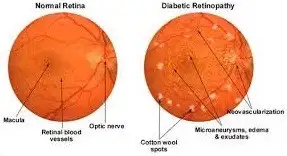
Diabetic retinopathy is a diabetes complication that affects eyes. It’s caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina). The cells in persons with diabetes mellitus have difficulty using and storing sugar properly. When blood sugar gets too high, it can damage the blood vessels in the rear of the eyes. This damage may lead to diabetic retinopathy. It can lead to vision loss or blindness. You already may have diabetic retinopathy, or be at risk for it. But you can take steps to reduce your risk of vision loss from this condition.
Diabetic retinopathy usually affects both eyes
Causes
The primary cause of diabetic retinopathy is diabetes — a condition in which the levels of glucose (sugar) in the blood are too high. Elevated sugar levels from diabetes can damage the small blood vessels that nourish the retina and may in some cases block them completely. As a result, the blood supply to the retina from these damaged blood vessels is cut off and vision is affected.
In response to the lack of blood supply, the eye may create growth factors that lead to diabetic macular edema, which can lead to decreased vision, or proliferative diabetic retinopathy, which can lead to retinal detachment and vision loss.
Causes
The primary cause of diabetic retinopathy is diabetes — a condition in which the levels of glucose (sugar) in the blood are too high. Elevated sugar levels from diabetes can damage the small blood vessels that nourish the retina and may in some cases block them completely. As a result, the blood supply to the retina from these damaged blood vessels is cut off and vision is affected.
In response to the lack of blood supply, the eye may create growth factors that lead to diabetic macular edema, which can lead to decreased vision, or proliferative diabetic retinopathy, which can lead to retinal detachment and vision loss.
Risk of developing diabetic retinopathy can increase as a result of:
Complications can lead to serious vision problems:
Vitreous hemorrhage by itself usually doesn’t cause permanent vision loss. The blood often clears from the eye within a few weeks or months. Unless your retina is damaged, your vision may return to its previous clarity.
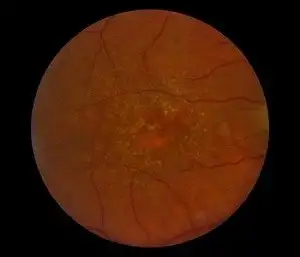
Diabetes damages the blood vessels of the Retina & as a result, they may leak fluid, proteins or fats or they may rupture & cause haemorrhage (bleeding) or they may get blocked. This is seen in Background Diabetic Retinopathy.
In the more severe cases, as the blood vessels get blocked, the subsequent loss of nutrition & oxygen to the retina promotes the growth, i.e. proliferation of new, fragile abnormal vessels on the optic disc or elsewhere which easily rupture & use cause large haemorrhage & severe visual loss or blindness. This is seen in Proliferative Diabetic Retinopathy.
When there is involvement of the central vision with difficulty in near vision affecting the most part of the retina called Macula it is known as Diabetic maculopathy.
The problem with diabetic retinopathy is that there are no symptoms in the early stages. During the time when retinopathy is most easily treated, the diabetic will not notice visual changes. In fact, more than 50% of patients with proliferative retinpathy may have good vision for 5 years or more. When visual symptoms start, it is often too late. Therefore, consider the following steps:
In addition to this exam, there are 3 other diagnostic tools eye specialist use to detect and manage diabetic retinopathy:
Fundus Photograph : This involves taking images of retina using a specialized non contact fundus camera.
Fundus Fluorescein Angiography (FFA): By injecting dye into one of the peripheral veins, severity of retinopathy can be picked up for treatment depending on the pattern of dye leakage.
Optical Coherence Tomography (OCT): is non-invasive as compared to FFA (no needle) & with fundus photography, it provides accurate screening for diabetic retinopathy severity. We have installed the latest 3D OCT at Ojas for enhanced imaging quality.
In addition, the eye doctor may:
Tags = Retina treatment in India, Retina specialist in India, Retina Surgery In Mumbai, best Retina hospital In Mumbai, Retina surgeon in Mumbai, Retina Specialist in Mumbai, Retina Treatment In Mumbai
You Can See My ppt By click this Link https://www.slideshare.net/drniteen00/bladeless-lasik-in-mumbai-ojas-eye-hospital