In the healthcare industry, the accuracy and efficiency of billing processes are critical for ensuring financial stability and operational success. Medical billing system software is a complex and time-consuming task that involves a series of steps, from patient registration and insurance verification to coding, claims submission, and follow-up on payments. A slight mistake at any stage can lead to claim denials, delayed reimbursements, and increased administrative costs. This can disrupt the revenue cycle and affect the overall financial health of healthcare organizations.
To address these challenges, healthcare providers are increasingly turning to advanced medical billing solutions that automate and streamline these processes. These solutions not only reduce errors and improve claim accuracy but also enhance operational efficiency and ensure timely reimbursements. With the right tools, healthcare providers can focus on delivering quality patient care while maintaining a smooth and profitable revenue cycle.
Automating the Billing Process for Better Efficiency:
Medical billing solutions offer a high level of automation that significantly reduces manual intervention in the claims process. These systems seamlessly integrate with Electronic Health Records (EHR) and Practice Management Systems (PMS), allowing for automatic data extraction and processing. This integration helps to eliminate human errors related to manual data entry, ensuring that claims are created with accurate patient information and service details.
Additionally, these solutions automate claims submission, ensuring that insurance claims are transmitted electronically and without delays. Automation reduces the time between service delivery and payment receipt, leading to faster reimbursements and improved cash flow. Healthcare providers no longer need to manually follow up on claims, as the system can track their progress in real time and flag any issues for immediate attention.
Enhancing Coding Accuracy and Compliance:
Accurate coding is essential for medical billing, as it directly influences reimbursement amounts. Incorrect coding can lead to underpayments, claim denials, or even legal and compliance issues. Advanced billing solutions come with built-in coding tools that automatically assign the correct medical codes (ICD-10, CPT, and HCPCS) based on the services provided and the patient’s diagnosis. This reduces the likelihood of coding errors and ensures that claims are compliant with the latest healthcare regulations.
These systems are updated regularly to reflect changes in coding standards and regulations, ensuring that healthcare providers remain compliant with federal and state laws. Automated coding verification also helps to minimize the risk of billing audits, which can be costly and time-consuming for healthcare organizations.
Simplifying Denial Management:
Claim denials are a common issue in medical billing, but managing denials effectively can minimize their impact. Advanced healthcare billing solutions include denial management tools that automatically identify and categorize denied claims. These systems generate reports to help providers understand the reasons behind claim denials and guide them through the appeals process.
By analyzing denial trends, healthcare organizations can identify recurring issues, such as errors in coding or payer-specific requirements, and make the necessary adjustments to prevent future denials. This proactive approach helps providers reduce administrative costs and accelerate the resolution of denied claims, ultimately improving their reimbursement rates.
Improving the Patient Billing Experience:
A major advantage of modern medical billing solutions is their ability to improve the patient billing experience. With clear and transparent billing, patients can easily understand their medical charges and payment responsibilities. Many billing solutions offer online patient portals where individuals can access their statements, review services rendered, and make payments securely.
The integration of online payment options allows patients to pay their bills conveniently, reducing the need for in-person visits or phone calls to the billing department. This not only enhances the patient experience but also improves the efficiency of payment collection for healthcare providers.
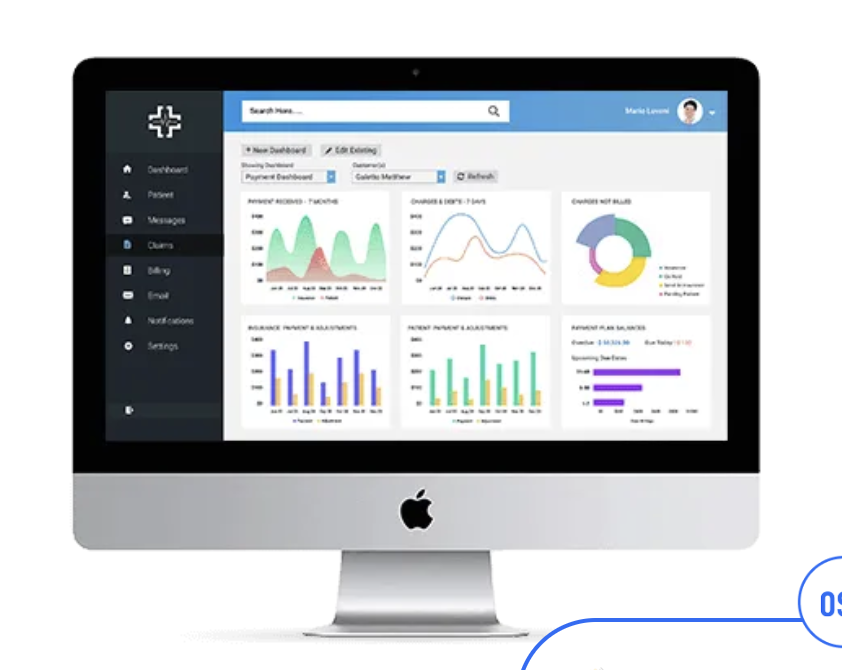
Real-Time Reporting and Analytics:
Medical billing solutions offer powerful reporting and analytics tools that provide healthcare providers with valuable insights into their revenue cycle. By tracking key metrics such as claim rejection rates, payment timelines, and payer performance, providers can identify areas where improvements are needed.
These insights help organizations make data-driven decisions that optimize their billing processes and enhance financial performance. Real-time reporting also enables providers to monitor the overall health of their revenue cycle, allowing them to take immediate corrective actions if necessary.
Conclusion:
In today’s complex healthcare environment, accurate and efficient medical billing is essential for financial success. Advanced medical billing software solutions are revolutionizing the way healthcare organizations manage their revenue cycle, improving efficiency, reducing errors, and accelerating reimbursements. By automating tasks such as claims submission, coding, and denial management, these systems help providers streamline operations, reduce administrative overhead, and improve cash flow.
Furthermore, these solutions enhance the patient experience by offering transparent billing and convenient payment options. With real-time reporting and analytics, healthcare organizations gain valuable insights into their financial performance, enabling them to make informed decisions and optimize their billing processes.
Adopting modern medical billing solutions is a smart investment for any healthcare provider looking to improve operational efficiency, ensure compliance, and achieve long-term financial sustainability.


 Australia
Australia India
India Singapore
Singapore United Kingdom
United Kingdom Germany
Germany South Africa
South Africa New Zealand
New Zealand Nigeria
Nigeria Canada
Canada France
France Spain
Spain Italy
Italy Ireland
Ireland UAE
UAE